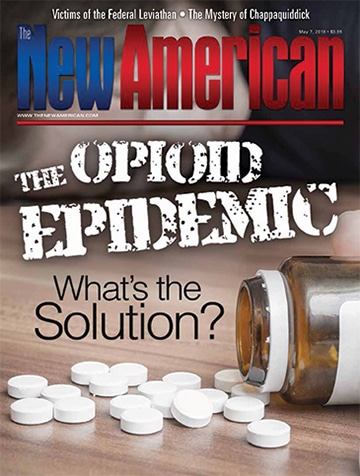
The Opioid Epidemic: What’s the Solution?
Foreign enemies are smuggling deadly poison across the border, killing record numbers of civilians. Instead of confronting the invaders, government and media demonize the nation’s physicians, blaming them for the catastrophic rise in death rate, while gagging a lone medical doctor who devised a brilliant yet inexpensive antidote to the poison. Sounds like the premise of a Hollywood suspense-drama, doesn’t it? Unfortunately, it is a factual summary of the current opioid epidemic crushing our country in its death grip.
Deaths from opioids have more than quadrupled in less than two decades. The Centers for Disease Control and Prevention (CDC) reports that nationwide, more than 42,000 of nearly 64,000 drug-overdose deaths in 2016 involved opioids. Late last year President Donald Trump declared it a public health emergency, and drug overdoses have become the leading cause of death for Americans under age 50.
How did this catastrophe happen? “It began in the late 1990s, when doctors and health care providers started facing pressure to treat chronic pain more aggressively,” declared The Hill in March. The Hill also blamed pharmaceutical companies for “marketing these drugs to medical providers as not addictive or harmful.”
JBS Member or ShopJBS.org Customer?
Sign in with your ShopJBS.org account username and password or use that login to subscribe.
 Subscribe Now
Subscribe Now
- 24 Issues Per Year
- Digital Edition Access
- Exclusive Subscriber Content
- Audio provided for all articles
- Unlimited access to past issues
- Cancel anytime.
- Renews automatically
 Subscribe Now
Subscribe Now
- 24 Issues Per Year
- Print edition delivery (USA)
*Available Outside USA - Digital Edition Access
- Exclusive Subscriber Content
- Audio provided for all articles
- Unlimited access to past issues
- Cancel anytime.
- Renews automatically