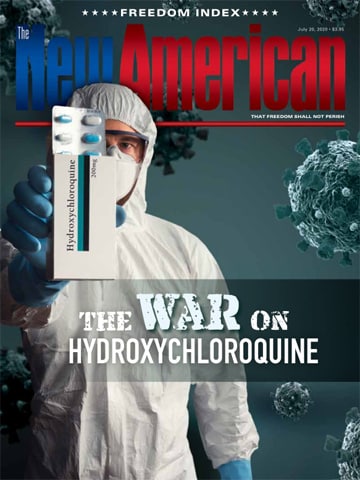
The Science of Hydroxychloroquine
It is one of the most commonly used drugs in the world. It has been available for decades and millions of people use it every day. Doctors recommend it to treat fevers in children and adults, and they suggest people use it post-surgery. There is good reason for this: It works, and in normal therapeutic doses is reasonably safe. But, like all drugs, there is a dark side to this one.
Because this drug is so readily available and so cheap, most people believe it is among the safest drugs they can take, yet overdoses, even mild ones, can lead to severe health problems. This tendency is exacerbated by the ready availability of extended release formulations that sometimes offer higher-than-normal dosing, making it easier to overdose. As a result, a shocking number of people are killed each year from misuse of this drug.
Writing for StatPearls, a peer-reviewed information source for healthcare professionals, researchers Suneil Agrawal and Babak Khazaeni noted that this drug “is the second most common cause of liver transplantation worldwide and the most common in the US. It is responsible for 56,000 emergency department visits, 2600 hospitalizations, and 500 deaths per year in the United States. Fifty percent of these are unintentional overdoses.”
JBS Member?
Sign in with your ShopJBS.org account.
 Subscribe Now
Subscribe Now
- 12 Issues Per Year
- Digital Edition Access
- Digital Insider Report
- Exclusive Subscriber Content
- Audio provided for all articles
- Unlimited access to past issues
- Cancel anytime.
- Renews automatically
 Subscribe Now
Subscribe Now
- 12 Issues Per Year
- Print edition delivery (USA)
*Available Outside USA - Digital Edition Access
- Digital Insider Report
- Exclusive Subscriber Content
- Audio provided for all articles
- Unlimited access to past issues
- Cancel anytime.
- Renews automatically