In 2007, a 63-year-old American veteran went to a VA hospital for evaluation of his exertional chest pain — again. Seven years earlier he had undergone an angioplasty to three of the arteries of his heart, and since then he had been treated for high blood pressure, high cholesterol, and fibromyalgia. In 2005, his chest pain had returned and now it was getting worse.
His doctors scheduled him for a nuclear study of his heart. He had had two of these tests over the previous two years, but each time they found nothing wrong. His doctors had told him that he needed another nuclear study — injecting him with radioactive material so that they could monitor his blood flow and the functioning of his heart — before they could run any other tests.
This would be his third study in two years. He was at the mercy of the system, so like any good soldier, he followed orders, but he was afraid his heart problem would be missed again.
The government’s protocol for performing such a test — the only correct way as far as the government is concerned — is dubbed the “two injection rest-stress approach.” First, a resting patient is given an injection of a radiotracer (in this case “sestamibi,” which contains the radioactive isotope technetium-99m). After the tracer has time to disperse throughout the heart and its arteries, imaging of the heart is done. When the radioactive material in the radiotracer has sufficiently decayed, the patient then exercises — or as doctors say, is “stressed” — and is given a second injection of a radiotracer to enable more imaging.
Failure to do the study any other way would result in repercussions, though numerous studies showed that this protocol was missing the most severe heart disease. In fact, every year between 70,000 and 130,000 Americans die because the government-supported method misses critical disease. That’s more than a million deaths in the last decade.
Fortunately for this patient, one of his doctors hadn’t been trained in the military, and was determined to perform the study based upon the best scientific evidence, honoring his Hippocratic oath.
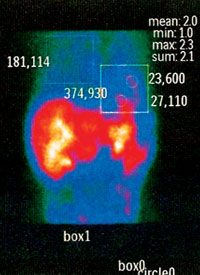
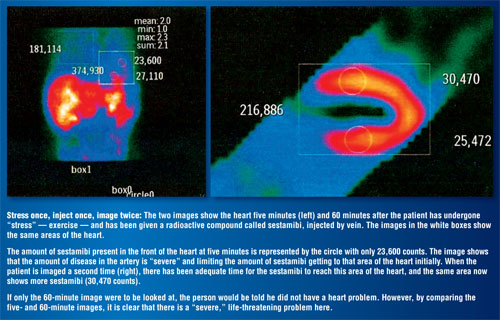
On the doctor’s part, dealing with the “system” while at the same time providing the best care possible would require patience: He needed to get his colleagues’ approval, as well as the patient’s and the people in the nuclear department. All this to merely change the test slightly — to “image” the heart twice after exercise, rather than doing it once (imaging it once five minutes after exercise and a second time 60 minutes after exercise). The five- and 60-minute “stress-stress” sequential images could then be compared. This comparison of stress tests, both the doctor and his colleagues believed, would show the hidden cause of his patient’s chest pain, if the “rest-stress” approach failed.
A New Standard of Care
When the veteran checked into the hospital, he was required to wear a heart monitor to continually keep track of his heart rate and any changes that might suggest problems with blood flow to his heart. His electrocardiogram (EKG) showed no evidence of him having problems with blood flow (ischemia) to his heart. His doctors were all well trained, and the hospital had the newest nuclear equipment, designed to unmask the errors seen with other SPECT (nuclear) cameras. The additional imaging he would undergo would not require more risk because it would not require submitting to more radiation. In fact, it would only require extra time needed to take another image of his heart.
 Again the rest-stress test showed no problems with his heart; no evidence of heart disease.
Again the rest-stress test showed no problems with his heart; no evidence of heart disease.
Efforts by the cardiologists to view the two “stress” images were delayed by the hospital staff, since only the rest-stress results were necessary, and only those results would be looked at by the radiologist. The cardiologists would be the only ones looking at the stress-stress results. Our veteran was told he was fine to go home.
As the veteran was getting dressed and preparing to go home, the cardiologists were finally able to look at the results of his five-minute and 60-minute images and discovered “critical” disease, including a major cause of death in people with heart disease: “vulnerable inflammatory plaques” (VIPs), which were ready to rupture. At that moment, the patient’s still-attached monitoring device suddenly alerted the nurses to what his cardiologists were seeing in the nuclear lab — the veteran was about to have a massive heart attack. Critical heart disease, indicated by chest pain signaling a life-threatening emergency, was completely missed by the rest-stress approach.
The five-minute image showed “critical” coronary artery disease that did not show up on the 60-minute image. It indicated a serious life-threatening problem missed by the rest-stress approach so vehemently supported by the government and its experts.
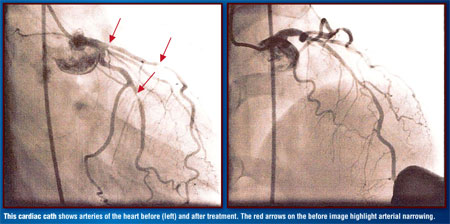
Aware of the findings from the stress-stress imaging, pioneered only years before, the team of cardiologists rushed our veteran to the cardiac catheterization laboratory where he was noted to have “critical narrowing” and “VIPs” in several arteries. (See cardiac cath images above.) This life-threatening scenario was treated with stents, and both his chest pain and the heart attack itself resolved.
This veteran finally received the “standard of care” he deserved, rather than the approach supported by the Department of Health and Human Services and by people who had inadequate knowledge of nuclear cardiology and the present scientific literature. Instead of being sent home, like so many others, this veteran had the right doctors at the right place at the right time. Because of this, our 63-year-old American veteran returned home to celebrate Christmas with his family. A Christmas he almost didn’t make.
And even the standard of care the veteran received was less than the best. There is no need for a second injection of radiotracer, which endangers the life of the patient — and costs lots of wasted money, including money for misdiagnosis errors. All that need be done is “stress” the person and give a single injection of the isotope, after which sequential images of the heart are taken five minutes and 60 minutes later and then compared to each other. This approach takes less time for the patient and uses less of our radioactive compounds, which should result in the test costing less. (This has been dubbed the Fleming Harrington Redistribution Washin Washout.)
What Went Wrong?
Every year, 10 million nuclear studies of the heart are performed. The current “rest-stress” approach accurately detects two-thirds of these. Of those missed, some 20 percent of patients have “critical” disease, resulting in the 70,000 to 130,000 deaths previously mentioned. These people succumb to sudden heart attacks after being told they do not have heart disease. Another 12 percent of people are told they have heart disease when they don’t. So it is reasonable to ask: Why are these studies so bad? And if they are so inaccurate, why should we even being wasting time doing them? The answer will surprise you — or maybe not.
The answer actually has its genesis in the history of nuclear cardiology. In 1927, Hermann Blumgart developed the first method for measuring the strength of the heart by injecting himself and others with a radioactive compound named radium C. Radium C was a combination of radioactive substances, the injection of which would probably have resulted in his being thrown in jail today. Dr. Blumgart demonstrated that the weaker the heart, the longer it would take for the radium C to travel from the veins on one side of the body to the arteries on the other side of the body. Assessing the travel time of radium C would require sequential measurement of change in the amount of radium C, which would be detected by a relatively impractical machine called a cloud chamber. By 1959, Richard Gorlin reinforced Blumgart’s method and pointed out that this sequential measurement had to be made under same-state conditions: “stress.” Gorlin also pointed out that “resting” images (used by many people today and supported by the government) were to be used only for detection of heart “damage” and not coronary artery (ischemia) disease.
By 1965, William Love showed that a Geiger counter placed over the heart could do sequential measurement in much the same way as Blumgart’s cloud chamber except that it was much more practical to use, but there was doubt as to whether a useful radioactive isotope would ever be developed that could be used routinely in patients. The introduction of Thallium-201 in the mid-1970s made such an isotope available, and testing began.
Using knowledge already garnered, a test was developed whereby a patient walked on a treadmill or pedaled on an exercise bicycle in an effort to “stress” the heart, after which Thallium-201 (Tl-201) was injected into a vein and circulated throughout the body, including the heart where it could then be seen using a SPECT (single photon emission computed tomography) camera. The first set of images had to be taken one hour after “stress” to allow for sufficient time for an adequate image of the heart to be taken. Using the approach laid out by Blumgart, Gorlin, and Love of comparing results over time, a second set of images following “stress” were taken three hours later. These two sets of images were compared to look for changes in isotope concentration over time. This difference was called “redistribution” and allowed physicians of the day to look for evidence of ischemia. For whatever reason, instead of calling these images “one” and “two,” or “one-hour” and “four-hour,” or “stress 1” and “stress 2” — or something equally logical — the first and second images obtained in this manner would later be called “stress” and “rest,” and the rest of the story, as is said, was history. The terms would stick, as would the problems they would create. From that point on out, many people and the government would be unable to think in terms other than rest-stress.
The Problem Grows
 Not only did nuclear testing procedures develop to match the terminology — rather than the terminology being developed to match the procedure — but problems with the radioactive isotope in use at the time and equipment weaknesses exacerbated bad results.
Not only did nuclear testing procedures develop to match the terminology — rather than the terminology being developed to match the procedure — but problems with the radioactive isotope in use at the time and equipment weaknesses exacerbated bad results.
The quality of images obtained with Tl-201 limited its usefulness and resulted in a search for newer and better radioactive isotopes, which by the late 1980s were becoming available, at least to those doing research.
One of the more useful of these new agents, sestamibi, redistributed slowly — remember, in a nuclear stress test, a radiotracer distributes in the heart in a manner proportional to blood flow, and if there is ischemia (or lack of blood flow), there should be a lower radioactive signal. Some people claimed that sestamibi was so slow at “redistributing” that it didn’t really redistribute at all. Of course, the U.S. government adopted this as its working hypothesis, though there were multiple studies already published showing this wasn’t true. Unfortunately, this led to much nuclear research being abandoned in the United States and instead being done outside of the United States. In 1988, Jean Maublant showed that sestamibi did in fact “redistribute,” and efforts were made to bring nuclear research to the United States. Then Quan-Sheng Li and Paul Crane both showed that the “redistribution” of sestamibi could be used to find coronary artery disease.
By 2000, though it was discovered that heart disease and breast cancer could be diagnosed simultaneously using the “redistribution” properties of sestamibi, it was evident that some part of the process was not functioning as it should. One patient would have more sestamibi redistributed at the time of the five-minute imaging than at the 60-minute imaging, and other patients would have more at 60 minutes than five minutes.
It turns out that the problem was with the SPECT cameras — they weren’t doing what we expected of them. Cardiologists were instructing their nuclear cameras to divide the information they receive from the heart into smaller and smaller pieces (more pixels) so that the picture looked “prettier,” but the increased pixels yielded false information.
For instance, if a SPECT camera, today’s modern Geiger counter, is used to measure how much radiation is coming from a syringe of sestamibi, it should show less and less radiation as the radioactive part of sestamibi goes through radioactive decay. The amount of radiation 55 minutes later should be only 90 percent of the radioactivity of the initial test, based upon the half-life of technetium-99m (Tc-99m), the radioactive component of sestamibi. This is easily seen when a SPECT camera breaks the image into a 64 by 64 matrix — the camera accurately measures the decay of Tc-99m. However, if the camera’s settings are changed to break the image into more pieces, e.g., a 128 by 128 matrix, which will include more lines between the pixels where the amount of radiation cannot be measured, the camera will lose five times as much data, giving the wrong results. In other words, the camera cannot accurately measure what it is seeing. This means that when we are using today’s SPECT cameras we must use the 64 by 64 matrix, or the results will be wrong.
We now know that comparing sestamibi “redistribution” (or redistribution of one of the other radiotracers such as Myoview) will not only tell us whether a person has heart disease, but will also tell us what we will see in the cardiac catheterization suite and allow us to more rapidly and correctly treat people, like our veteran. You would think the government would embrace this approach, particularly if it’s going to practice medicine, but it doesn’t.
Third World U.S. Healthcare?
Today, more than a decade after my colleagues and I and others confirmed that sestamibi redistribution is real and how important this is to the detection of VIPs, and to helping diagnose and treat “critically” ill individuals, there is still no news of it being used in the United States.
Despite the publication of our findings two years ago in the DeBakey Medical Journal, multiple publications in the Australian/New Zealand Nuclear Medicine Journal, presentations in Europe and the United States, last year’s publication in The Federal Practitioner (the U.S. government’s own peer-review medical journal), and support for our findings by publications at UCLA and Harvard, as well as other investigators and clinicians from around the world, and recent additions in Medline-Plus (the website for the National Institute of Health and the National Library of Medicine) changing the information on its website to incorporate our work, there has been no change by HHS or any other government agencies’ policies. Instead of allowing American physicians to improve the field of medicine and the quality of healthcare provided in the United States, just as we did with the veteran above, I see a recalcitrant system that appears to be less interested in American physicians and American healthcare than its own ego.
It is as if the U.S. government doesn’t accept the realization that medicine is a constantly evolving discipline, though it has been evolving steadily for generations. In 1850, Ignaz Philipp Semmelweis tried to explain that by washing hands between each delivery of a child, physicians could reduce infant mortality. The system believed he was wrong, because everyone knew that infections were due to “humours,” not bacteria. When Archie Cochrane was a POW in Germany during WWII, he discovered that much of what was considered traditional practice in the realm of medicine was not based on scientific fact and, indeed, resulted in poorer outcomes than what he was able to provide using the limited supplies the Nazis gave him. In fact, Archie Cochrane lost only four people during the entire time he cared for his fellow prisoners, while the best British hospitals in London lost more than that each day, though they treated patients with similar ailments.
The efforts by the U.S. government today are reminiscent of Archie Cochrane’s day. When Archie asked the German Stabsarzt for more doctors to help him care for the ill, they replied “Nein! Aerzte sind ueberfluessig.” (No! Doctors are superfluous!) It seems that this is what we are being told today. When I go elsewhere in the world and present our findings, the work is welcomed and applied. Here, there is no such welcome by the government.
When I entered medical school at the University of Iowa in 1981, the Dean of the Medical School told our class that 90 percent of what we would be taught would be wrong, and he encouraged those of us who wanted to make a difference to try to find out what was wrong and help improve healthcare. Since then, that is what I have spent my life doing. He forgot to tell us that there would be those who for a variety of reasons would try to prevent us from doing this. My only question is why the U.S. government or anyone else would play such a role in prohibiting Americans from getting better healthcare.
In June of 2011, I will be presenting this important work at the Society of Nuclear Medicine meetings in San Antonio, Texas, and one of my colleagues will be presenting other work at the Health Physics Society meetings in Florida. We have been asked (and have done so) to submit our work to the International Atomic Energy Administration, and the U.S. government would appear to be cognizant of what we are saying, without doing anything about it. While other countries, including Iran, are publishing similar work, our discoveries are ignored here. Will it soon be possible to get better healthcare in Iran?
Dr. Richard M. Fleming is an American-born and -trained nuclear cardiologist. He is the founder of the “Inflammation and Heart Disease” theory and the Fleming Harrington Redistribution Washin Washout method of cardiology testing.



